Golfing. Gardening. Strolling along the beach. Many of our favorite moments take place under the sun. But while memories may fade, your skin doesn’t forget—and every moment of unprotected sun exposure adds up.
Over time, this exposure can cause what dermatologists call actinically-damaged skin—visible signs of UV-induced damage that may lead to precancerous skin lesions known as actinic keratoses (AKs). And with over 58 million cases in the U.S., it’s one of the most common skin conditions in adults.
So, what does actinic keratosis look like? And how can you help protect your skin? With guidance from expert dermatologists, we’ll explore the causes, appearance, prevention, and treatment of AKs.

Dr. Susana Puig
World-renowned dermatologist in the field of diagnosis and treatment of melanoma and skin cancer. Professor at the University of Barcelona.

Dr. Caroline Robinson
Chicago-based, board-certified medical and cosmetic dermatologist with subspecialty expertise in alopecia, preventative skincare, and ethnic skin dermatology.

What is actinic keratosis or actinic damage?
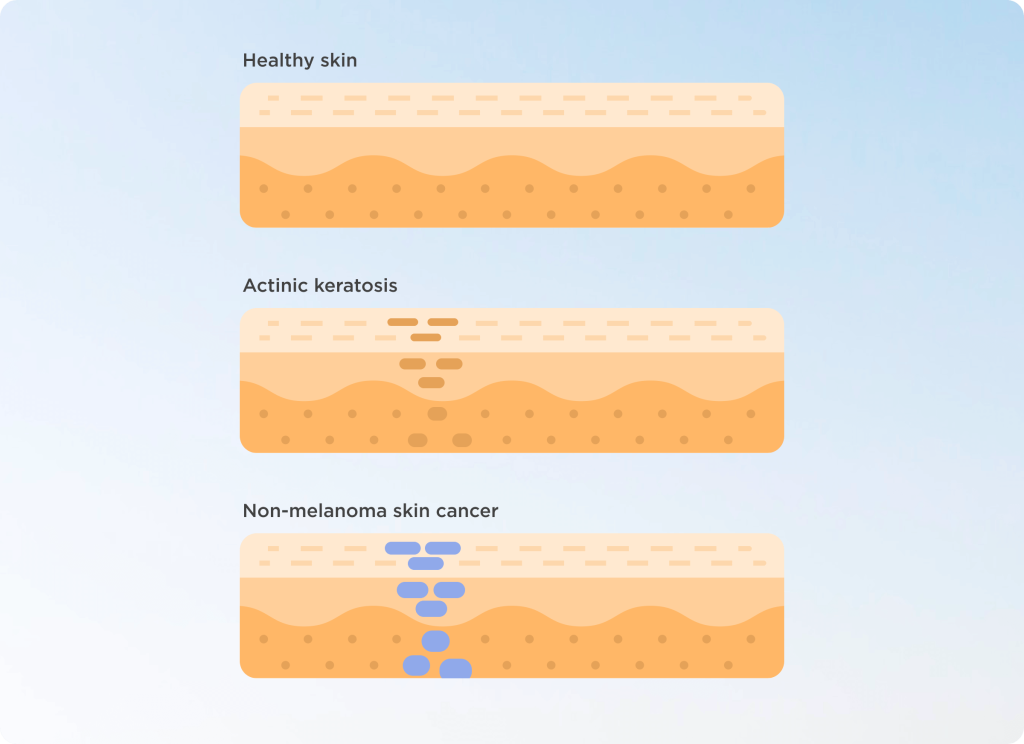
Actinic keratosis—also known as solar keratosis—is a small, rough, often scaly patch on the skin caused by cumulative sun exposure over time. While AKs are not skin cancer themselves, they are considered precancerous lesions that have the potential to develop into squamous cell carcinoma (SCC), a common type of skin cancer.
Although most of the time they’re nothing to worry about, it’s estimated that around 10% of actinic keratoses can progress to skin cancer—making early detection and regular visits with your dermatologist essential.
At least 90% of actinic keratoses are benign—meaning they will not turn into cancer.
What causes actinic keratosis?
Short answer: the sun. The main culprit is ultraviolet (UV) radiation—from spending time outdoors or artificial sources like tanning beds. Repeated and unprotected exposure to UV light damages skin cells over time, creating changes in their DNA. This cumulative harm leads to the formation of actinically damaged skin, which may appear as AKs.
Common risk factors include:
- Light skin tones (Phototypes I–II)
- Long hours outdoors (work or leisure)
- History of sunburns, especially in childhood
- Use of tanning beds
- Age over 40
In short, anyone with a history of sun exposure—especially without daily sun protection—may develop AKs.
Expert tip: While medical experts have contributed to and fact-checked this article, there are lots of additional sources of data on actinic keratosis available. Turn to these foundations for the latest information:
American Academy of Dermatology
Skin Cancer Foundation
Yale Medicine
What does actinic keratosis look like?

AKs can be easy to miss. They tend to start off as a patch of rough or scaly skin, with a pink or red color. But keep in mind that they can present differently in different people.
Here’s what to watch for:
- Rough or scaly texture- Typically described as feeling like sandpaper. AKs can often be mistaken for warts, sun spots, or dry patches—but their rough texture is often a giveaway.
- Color variations- Patches may be pink, red, brown, or skin-toned.
- Size and shape- Typically small (less than 2.5 cm), flat, or slightly raised.
- Persistent dry spots- Especially those that don’t heal or flake repeatedly-
And where to look:
- Face and scalp- AKs frequently appear on the face and bald scalp, two areas often exposed to sunlight.
- Backs of the hands- Constant sun exposure makes this another high-risk area.
- Lips- A white, cracked, or scaly patch on the lower lip may point to a form of AK.
If you notice any of these signs—especially in areas with frequent sun exposure—it’s a good idea to schedule a checkup with your dermatologist.
How can I help prevent actinic keratosis?

Step 1: Use sun protection every day
Here’s the good news: you can take proven steps to reduce your risk. Dr. Puig confirms, “Daily sun protection helps minimize the risk of skin damage and cancer.” And it’s as simple as following a few easy sun safety tips:
- Apply a broad-spectrum sunscreen with SPF 30 or higher daily—yes, even when it’s cloudy
- Reapply at least every 2 hours, especially after swimming or sweating
- Wear hats, sunglasses, and protective clothing when possible
- Do your best to avoid peak sun hours (usually 10 AM–4 PM)
Expert tip: Dr. Puig echoes the importance of applying sunscreen the right way, “We must apply a sufficient amount of product and distribute it correctly.” That means paying extra attention to those easy-to-miss and AK-vulnerable spots like your ears, nose, and backs of your hands.
Opt for sunscreens that do more
Sunscreen is your first line of defense—but certain formulas do more. Dr. Weisert recommends Eryfotona Actinica and Eryfotona Ageless featuring DNA Repairsomes® to help protect skin and repair past damage. “[They’re] 100% mineral-based sunscreens that are dermatologist tested,” she shares.

But the formula isn’t the only thing that matters. Dr. Weisert continues, “I always tell my patients that the best sunscreen is one that they’re actually going to wear.” Consistent use is key, and an easy-to-wear texture can make all the difference. “What I love about the Eryfotona line is that they’re ultra-lightweight and apply seamlessly onto the skin.”
View this post on Instagram
“Both Eryfotona Actinica and Eryfotona Ageless contain DNA Repairsomes®, which help to repair existing sun damage.”
– Dr. Elise Weisert
Step 2: Perform regular skin self-exams
While self-exams can’t diagnose actinic keratosis or replace your yearly visit to the dermatologist, they can help you be proactive.
Here’s what to look for:
- Persistent redness or dryness in sun-exposed areas
- New rough patches or scaly areas
- Spots that change in shape, size, or color
Expert tip: Take notes or pictures on your phone to track any changes. That way, you’ll be better prepared to discuss any concerns with your dermatologist when your appointment comes around.
How do you treat actinic keratosis?
The first step: get your dermatologist involved. It’s a good idea for everyone to check in with their dermatologist once a year. However, people with more skin cancer risk factors might need more frequent visits.
If you’re diagnosed with actinic keratosis at one of these checkups, rest assured that there are a variety of treatment options. The most common include:
- Cryotherapy
- Topical treatments
- Photodynamic therapy (PDT)
- Laser therapy or curettage
Something else to keep in mind: Even if your dermatologist treats visible lesions, AKs often occur in clusters, and areas of invisible damage may also exist. That’s why ongoing sun protection and regular skin exams are so important.
Listen to your skin

AKs are common—but they’re also preventable and treatable. The most powerful thing you can do? Keep paying attention. Your skin gives you signals. And when you protect, examine, and nourish it every day, you’re giving it the care it deserves.
Remember these three essentials:
- Use sunscreen daily (rain or shine)
- Perform self-checks frequently
- Visit your dermatologist yearly
Protect what protects you. Because your skin remembers it all—today, tomorrow, and yesterday.
References:
1 Actinic Keratosis (AK). (2022). Yale Medicine. https://www.yalemedicine.org/conditions/actinic-keratosis
2 The Skin Cancer Foundation. (2023, March 6). Squamous Cell Carcinoma – The Skin Cancer Foundation. https://www.skincancer.org/skin-cancer-information/squamous-cell-carcinoma/
3 Venosa, A. (2022). Is Actinic Keratosis Skin Cancer? What You Need to Know About this Common Condition. The Skin Cancer Foundation. https://www.skincancer.org/blog/is-actinic-keratosis-skin-cancer/


